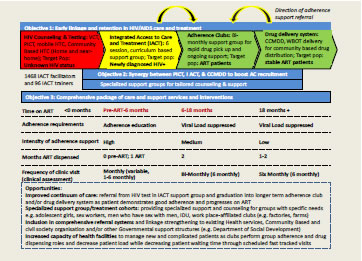
In the month of April, significant developments have been achieved within I ACT, specifically regarding the integration/collaboration of TA’s community projects, namely CBCT, I ACT and Adherence Clubs. This integration aims to create a comprehensive care and support package that is patient-centric and aims to improve adherence & retention in care from point of diagnosis and pre-initiation on ART, but also through initiation on ART and extending further to 18+ months stable on ART. The process begins where newly diagnosed HIV+ individuals (CBCT referrals) will be referred to I ACT, which then forms the education stage. This is where newly diagnosed individuals will receive key information on their diagnosis over 6 sessions, each session focussing on unique topics that will empower and allow these individuals to advocate for their own health care. This will essentially create a firm foundation based on the premise that sufficient knowledge creation will benefit the newly diagnosed individual to the extent that he/she continues to access services at the health care facility. Linked to this is the fact that the newly diagnosed individual will undergo these sessions in a support group setting where they can interact and share with peers that may be experiencing similar challenges all of which is facilitated by a trained IACT facilitator. Once these individuals have been stable on treatment for a period of 6 months and their viral load has been suppressed to lower than detectable limits they will then qualify to be enrolled in an ART Adherence Club.
In the club setting, groups of 20 stable ART patients meet bi-monthly. During one-hour club meetings patients receive observational assessments; peer support and pre-packed two-month supply of ART medication. Patients reporting symptoms suggesting illness, adverse drug reactions or weight loss are referred back for assessment to the clinic nurse. This reduces clinic visits for patients from 12 to 6 months. The design of ACs is that adherence to treatment (ie: not defaulting treatment and a viral load that is lower than detectable limits) yields an incentive to the patient who now only needs to return to the healthcare facility every 2 months as opposed to monthly. The individual remains in a club for a period of 12-18 months after which they are referred out of the facility to the nearest CCMDD site or other community initiatives like ward based outreach teams. At this stage the individual now has the benefit of collecting their medication every 2 months from a registered collection point within the community.
Piloting of IACT/Adherence Club integration is planned to start in May. Provision has been made through the Adherence Club Global Fund grant to place 11 I ACT facilitators in 11 health care facilities currently running Adherence Clubs. The aim is not only to have both projects implemented in one facility but to focus on the linkage from referral (CBCT) into I ACT (newly diagnosed) through to Adherence Clubs (stable on treatment) thereby improving patient retention and adherence over a prolonged period of time.
Below is an outline of the proposed integration of the projects: